Medicaid Nursing Home Payment Statistics
March 5, 2025
Explore Medicaid nursing home payment stats: dissecting rates, impacts, and strategies for managing payments.


Understanding Medicaid Nursing Home Payment Statistics
As one delves into the realm of Medicaid nursing home payment statistics, it becomes evident how crucial Medicaid is in facilitating payments for nursing home care. This section sheds light on the significance of Medicaid in nursing home payments and provides an overview of the statistics surrounding these payments.

Importance of Medicaid in Nursing Home Payments
Medicaid plays a pivotal role in supporting nursing home payments for individuals who require long-term care but may not have the financial means to cover the costs independently. For many elderly and low-income individuals, Medicaid serves as a lifeline, providing access to necessary nursing home services that would otherwise be financially out of reach.
Overview of Nursing Home Payment Statistics
Nursing home payment statistics offer valuable insights into the financial landscape of long-term care facilities and the role played by Medicaid in sustaining these services. By analyzing these statistics, policymakers, healthcare providers, and stakeholders can better understand the distribution of funds, average payment per resident, and the broader impact of Medicaid reimbursements on nursing home finances.

By comprehending the nuances of Medicaid nursing home payment statistics, stakeholders can identify trends, challenges, and opportunities for improvement within the long-term care system. Understanding these numbers is crucial for ensuring the financial sustainability of nursing homes and maintaining the quality of care provided to residents.
Factors Influencing Medicaid Payments
When it comes to Medicaid payments for nursing home care, several factors come into play, impacting both the rates of payment across states and the eligibility criteria for individuals seeking coverage.

State Variations in Payment Rates
Medicaid payment rates for nursing home care can vary significantly from state to state. These variations are influenced by factors such as state budgets, demographics, cost of living, and prevailing reimbursement models. It's important to note that disparities in payment rates can affect the quality of care provided in nursing homes, as facilities in states with lower payment rates may struggle to maintain high standards of care due to financial constraints.

Understanding the differences in payment rates among states is crucial for policymakers, healthcare providers, and individuals relying on Medicaid for nursing home coverage to advocate for fair and sustainable reimbursement practices.
Medicaid Eligibility Criteria for Nursing Home Coverage
Medicaid eligibility criteria for nursing home coverage play a significant role in determining who qualifies for financial assistance for long-term care. These criteria typically consider factors such as income, assets, medical necessity, and residency status. Individuals must meet specific financial and health-related requirements to qualify for Medicaid coverage of nursing home services.
It's essential for individuals and families planning for long-term care to understand the Medicaid eligibility criteria in their state to ensure they meet the necessary qualifications for coverage. Moreover, policymakers and advocacy groups often review and advocate for changes to these criteria to expand access to Medicaid coverage for those in need.
By considering both state-specific payment rates and eligibility criteria, stakeholders can work towards improving the Medicaid reimbursement system for nursing home care, ensuring equitable access to quality long-term care services for all individuals in need.
Breaking Down the Numbers
When it comes to understanding Medicaid nursing home payment statistics, analyzing the average Medicaid payment per resident and the distribution of Medicaid funds among nursing homes plays a crucial role in assessing the financial landscape of long-term care facilities.

Average Medicaid Payment per Resident
The average Medicaid payment per resident serves as a key indicator of the financial assistance provided to individuals in nursing homes. This metric reflects the amount of Medicaid funds allocated to cover the costs of care for each resident. By examining this figure, policymakers and healthcare providers gain insights into the level of support available for individuals relying on Medicaid for long-term care.
Distribution of Medicaid Funds among Nursing Homes
Understanding the distribution of Medicaid funds among nursing homes sheds light on the allocation of financial resources within the long-term care sector. This analysis reveals how Medicaid payments are distributed across different facilities, highlighting disparities in funding and resource allocation. By examining this distribution, stakeholders can identify trends, disparities, and areas for improvement in the equitable distribution of Medicaid funds.
To provide a comprehensive overview, let's delve into the numerical data related to these key aspects of Medicaid nursing home payments:

By breaking down these numbers, stakeholders can gain a deeper understanding of the financial dynamics at play within the Medicaid nursing home payment system. Analyzing these metrics is essential for policymakers, healthcare providers, and advocates working to enhance the quality of care, address financial challenges, and ensure the sustainability of nursing home facilities that rely on Medicaid funding.
Challenges and Implications
When delving into the realm of Medicaid nursing home payment statistics, it becomes evident that several challenges and implications arise from the intricacies of these financial matters. Two key aspects that significantly impact the landscape are the effect of Medicaid payment rates on care quality and the financial sustainability of nursing homes.
Impact of Medicaid Payment Rates on Care Quality
The payment rates set by Medicaid play a critical role in determining the level of care that nursing home residents receive. Lower reimbursement rates can put pressure on nursing homes to cut costs, potentially leading to staffing shortages, reduced quality of care, and compromised resident outcomes.
It is crucial to recognize the delicate balance between Medicaid reimbursement rates and the quality of care provided in nursing homes. Insufficient payment rates can hinder facilities from offering comprehensive services, adequate staffing levels, and necessary resources, ultimately affecting the well-being and satisfaction of residents.
Financial Sustainability of Nursing Homes
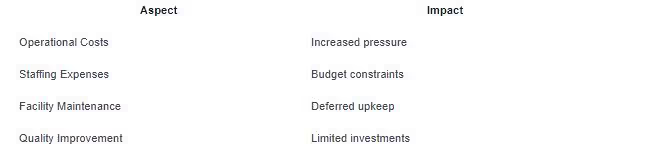
The financial sustainability of nursing homes hinges on various factors, with Medicaid payment rates being a significant determinant. Adequate reimbursement is essential to cover operational costs, staffing expenses, facility maintenance, and investments in quality improvement initiatives.
When Medicaid payment rates fall short of covering the actual costs of care, nursing homes may struggle to maintain financial stability. This can lead to operational challenges, limited resources for resident care, and, in severe cases, closures of facilities that serve vulnerable populations.
Navigating the complexities of Medicaid nursing home payment statistics is essential for understanding the broader implications on care quality and the financial viability of long-term care facilities. As policymakers, healthcare providers, and stakeholders assess these challenges, it is imperative to prioritize sustainable funding models that ensure the delivery of high-quality care to those in need within nursing home settings.
Strategies for Managing Medicaid Payments
When it comes to navigating the complexities of Medicaid nursing home payment statistics, individuals and institutions involved in long-term care must consider strategic approaches to manage these payments effectively. Two key strategies for managing Medicaid payments include Medicaid planning for long-term care and advocating for policy changes in Medicaid reimbursements.
Medicaid Planning for Long-Term Care
Medicaid planning for long-term care involves a proactive approach to financial and healthcare decision-making to ensure eligibility for Medicaid coverage for nursing home services. By engaging in Medicaid planning early on, individuals can strategically structure their assets and income to meet Medicaid's financial requirements without compromising their access to necessary care.
One crucial aspect of Medicaid planning is understanding the eligibility criteria and financial thresholds set by Medicaid for nursing home coverage. Through careful planning and consultation with financial advisors and elder law attorneys, individuals can navigate the Medicaid application process and optimize their financial situation to secure necessary long-term care services.
Advocating for Policy Changes in Medicaid Reimbursements
Advocating for policy changes in Medicaid reimbursements is another important strategy for managing Medicaid payments in the context of nursing home care. By actively engaging with policymakers, advocacy groups, and healthcare associations, stakeholders can work towards improving Medicaid payment rates, reimbursement methodologies, and overall support for long-term care facilities.
One of the primary goals of advocating for policy changes in Medicaid reimbursements is to address the financial challenges faced by nursing homes in providing quality care to Medicaid beneficiaries. By advocating for fair and adequate reimbursement rates, stakeholders can help ensure that nursing homes have the resources needed to maintain high standards of care, support staff, and invest in essential services for residents.
By implementing these strategies for managing Medicaid payments, individuals and organizations involved in long-term care can navigate the complexities of Medicaid nursing home payment statistics more effectively. Through proactive planning and advocacy efforts, stakeholders can work towards improving the financial sustainability of nursing homes, enhancing care quality, and ensuring access to essential services for vulnerable populations.
Sources
https://www.elizabethtownhcc.com/post/medicaid-nursing-home-payment-statistics
https://www.downersgrovehc.com/blog/does-medicaid-pay-for-assisted-living



























































.jpeg)











































































































































































































.avif)























































.jpeg)

































































.jpeg)














.jpg)









































.jpeg)








































































.avif)




.avif)

















































.avif)







































































































































































